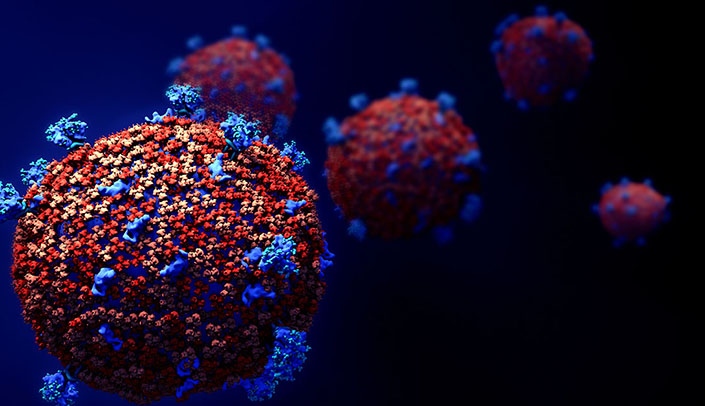
Senior care facilities place a high priority on person-centered care and attending to the body, mind, and spirit of the whole resident. One critical facet of that care is skin health and wound management. The good news is that there are more technologies and treatments, as well as certification and training programs, to help maximize outcomes and quality of life.
Find out more by going to https://www.providermagazine.com/Issues/2023/Winter/Pages/Strengthening-the-Chain-of-Wound-Prevention-and-Care.aspx