You can make a difference in how we understand the health care workforce who cares for people living with dementia across the United States.
Tag: dementia
Cure or Treatment for Dementia by 2025
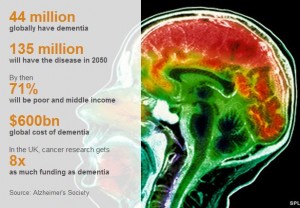
The NY Times didn’t cover it; neither did the Washington Post or the Wall Street Journal. But the BBC made a big deal of the G8 “dementia summit,” hosted by the UK just a month ago. Representatives from the research world, the pharmaceutical industry, and the Organization of Economic Development, along with government health leaders, met to discuss what to do about Dementia.
Almost all the members of the G8 took the conference seriously: the UK, Canada, France, Germany, Italy, Japan, and Russia each sent their top health representative. The US didn’t send the Secretary of Health and Human Services or an assistant secretary. The US sent the “acting assistant secretary for planning and evaluation” in the Department of Health and Human Services. This says it all: the US didn’t regard this conference as a priority.
What is Dementia?
- It is an umbrella term that describes about 100 diseases in which brain cells die on a huge scale.
- All damage memory, language, mental agility, understanding and judgement.
- Alzheimer’s disease is the most common form, affecting 62% of those living with dementia.
- It gets worse with time and eventually people are left completely dependent on carers.
- It is incurable
Dementia across the Globe
Reference:
Murriel Gillick, “The Latest War”,
http://blog.drmurielgillick.com/2014/01/the-latest-war.html
Perspectives On Aging
Showing We Care
Since the 1990s, physicians and patients have been fighting over futility. The doctors look at a patient who is dying and say that further tests and treatment cannot possibly work and shouldn’t be done. The patients, or more commonly their families, look at those same patients and say that they want “everything done” to try to prolong life.
As often happens in the US, the futility battle ended up in the court room. In the case of Helga Wanglie, an 86-year-old woman in a vegetative state after hip surgery, the doctors went to court over whether the patient’s husband had the right to insist that she remain on a ventilator. The court, as also often happens, didn’t address the issue of whether the ventilator was or was not appropriate treatment for Mrs. Wanglie; it simply ruled that her husband, as her surrogate, had the right to make the decision. After that case, many physicians concluded that the fight over futility was itself futile. For the last 15 years, physicians have tried to focus on determining a patient’s goals of care and then suggesting what treatments are most consistent with those goals. When they still cannot agree with family members about the right course of action, they resort to mediation, sometimes provided by a hospital ethics committee. But simmering below the surface, conflicts over perceived futility rage bubble vigorously.
A short article in the New England Journal of Medicine, “The Debt of Life—Thai Lessons on a Process-Oriented Ethical Logic,” offers a refreshing way of looking at futility. Based on his experiences doing ethnographic field work in Thailand while a graduate student in Anthropology, physician Scott Stonington shines a new light on the typical ICU dilemma. The physicians, he reports, are loathe to perform various possible tests and treatments because they think in terms of outcomes. They argue that their interventions won’t work in the sense that they won’t overcome the existing medical problems and that they are burdensome to the patient and, parenthetically, expensive. The patient’s family, he observes, think in terms of the process of care. He comments on one Thai family who said that their father had given them “flesh, blood, and breath” so they had a “debt of life” to pay. The ICU, they reasoned, allowed them to repay their debt: it gave their father flesh (tube feedings for nutrition), blood (intravenous medications and dialysis to cleanse the blood), and breath (a ventilator for breathing). The family was not so much interested in the outcome of treatment as in the treatment itself. In this scenario, the conflict was ultimately resolved when the family came to the conclusion that they had paid their debt and further aggressive care could be discontinued.

I made a very similar argument in my essay, “The Standard of Caring: Why Do We Still Use Feeding Tubes in Patients with Advanced Dementia?” I noted that it had been over 10 years since a series of studies in the medical literature reported that feeding tubes (a tube inserted into the stomach to provide nutrition) did not prolong life in patients with advanced dementia who had eating difficulties. These patients are nearing the end of their lives and no matter what procedures they have, their prognosis remains pretty much the same. Not only don’t the tubes prolong life, but they don’t accomplish a variety of other goals that doctors had hoped they might: preventing pressure ulcers (skin breakdown that is often related to malnutrition) or preventing pneumonia (caused by food going into the lungs instead of the stomach). As a result of these studies, the rate of tube feeding people with advanced dementia has declined, but it is still far from zero. I suggest that the reason some families want a feeding tube is to show that they care. It’s not that they expect to improve some quantifiable outcome—living longer or avoiding pneumonia. It’s that they want to have a way to demonstrate caring. For the same reason, we keep people with advanced dementia clean and dressed. We don’t require a study that shows that they will be less likely to develop an infection if they are kept clean. We don’t demand proof that they will live longer if they are clothed. We assume that being clean and clothed contribute to well-being because they are among the only ways we as caregivers have of showing respect for the human being who happens to have dementia. Tube feeding, from this perspective, is a means of proving that we care.
Resource:
Murriel Gillick, “Showing we care”, http://blog.drmurielgillick.com/2013/11/showing-we-care.html