The Role of Infection Control
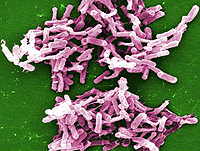
Standard teaching is that Clostridium difficile infection (CDI) is a hospital-acquired infection that reflects a failure of infection control, but it may be more closely related to antibiotic control. A recent report from the Centers for Disease Control and Prevention (CDC), based on an analysis of 10,342 cases of CDI in 111 hospitals and 310 nursing homes, showed that 75% of the patients were already colonized with C difficile at the time of admission.[1] Nearly all (94%) of these cases were “healthcare-associated,” meaning that acquisition occurred during an outpatient visit, a nursing home stay, the current hospitalization, or a previous hospitalization. Only 25% of patients actually acquired the pathogen in the same hospital where clinical expression of CDI occurred.
Clinical relevance. The CDC study suggests that infection control personnel and physicians need to be aware of this association, because this may require changes in infection control practice. The implication is that to prevent CDI, clinicians need to find ways to identify patients who are already colonized to protect them from obvious risks, and also to consider them to be potential sources of infection to others. This could substantially change infection control practice for prevention of CDI.
Fidaxomicin- Fidaxomicin is the second drug approved by the US Food and Drug Administration (FDA) for the treatment of CDI. The first was oral vancomycin, which was approved in 1978 on the basis of a 16-patient randomized controlled trial.[2] The fidaxomicin trials included approximately 1200 patients randomly assigned to receive fidaxomicin vs oral vancomycin.[3,4] Results showed similar initial response rates (88% vs 86%), but a significantly reduced rate of relapse in fidaxomicin recipients (15% vs 25%).[3] A subsequent trial showed that fidaxomicin was also superior to vancomycin in prevention of a second relapse in patients who had already experienced a relapse of CDI (36% vs 20%).[5] The presumed mechanism for reduced rates of relapse is a less pronounced alteration of the colonic microbiome with fidaxomicin,[6] which is presumed to be the ultimate control of C difficiletoxin production.
Clinical relevance. It appears that fidaxomicin is a good drug for CDI because it is FDA-approved; similar to oral vancomycin with respect to cure rates; and clearly superior in terms of “global cure” rates, which include initial responses without relapses. Nevertheless, the cost of fidaxomicin (which reflects the high cost of FDA trials) is intimidating.
Read More here – http://www.medscape.com/viewarticle/809238?nlid=33126_785